| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Original Article
Volume 11, Number 2, June 2022, pages 27-32
Disparities in Post Cesarean Section Pain Management
Alison Wilesa, b, Electra Korna, Cheryl Dinglasa, Beth Bentleya, Jonathan Rosnera, Salma Rahimia
aDepartment of Obstetrics and Gynecology, Mount Sinai South Nassau, Oceanside, NY, USA
bCorresponding Author: Alison Wiles, Department of Obstetrics and Gynecology, Mount Sinai South Nassau, Oceanside, NY 11570, USA
Manuscript submitted February 1, 2022, accepted April 7, 2022, published online June 16, 2022
Short title: Post Cesarean Section Pain Management
doi: https://doi.org/10.14740/jcgo786
| Abstract | ▴Top |
Background: Racial and ethnic disparities exist across all fields of healthcare, especially regarding assessment and treatment of pain. English language proficiency is a less frequently considered and studied aspect contributing to healthcare inequities. We evaluated if the frequency of pain assessment, severe pain scores, and medication administration after cesarean delivery differed by patient race and ethnicity and primary language in women after cesarean delivery at our hospital.
Methods: We performed a retrospective cohort study of all women who underwent cesarean birth resulting in a liveborn neonate at a single institution between January 1, 2018 and June 30, 2018. Pain scores documented and medications administered after delivery were grouped into 0 - 24 and 25 - 48 h postpartum time periods. Number of pain scores recorded, whether any pain score was 7 - 10 out of 10, and type and amounts of analgesic medication including non-steroidal anti-inflammatory drugs (NSAIDs) and oxycodone therapeutic equivalents (OTEs) were evaluated.
Results: The number of pain assessments was lowest in Hispanic and non-English speaking patients. No differences were observed in pain scores ≥ 7 between groups by race and ethnicity or primary language. NSAID doses were lowest in non-English speaking patients at 0 - 24 (P < 0.05) and 25 - 48 h (P < 0.05) postpartum and in black patients at 25 - 48 h postpartum (P < 0.0009). OTE doses were similar between groups by race and ethnicity and primary language at 0 - 24 h postpartum. OTE doses were lowest in Hispanic and non-English speaking patients and highest in black patients at 25 - 48 h (P < 0.05).
Conclusions: Racial, ethnic, and language-related inequities in postpartum pain assessment and treatment were found in our study. The exact cause of these disparities remains unclear. Further work can be done through standardization of postpartum order sets to eliminate these disparities.
Keywords: Post-operative pain; Racial disparities; Ethnic disparities; Narcotic; NSAID; Pain assessments
| Introduction | ▴Top |
Evidence of racial and ethnic disparities is consistent and pervasive across all of healthcare and has persisted despite public health and medical advances. In 2003, the Institute of Medicine’s Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care reviewed numerous studies and found that racial and ethnic minorities receive lower quality care than nonminority groups. They also found that these differences persisted even with adjustment for access-related factors [1]. Racial and ethnic disparities in pain management have been well documented in the literature from emergency departments, to outpatient clinics, to obstetric analgesia [2-4]. Emerging data suggest postpartum pain management has similar disparities [5, 6]. There have also been well documented disparities in perinatal outcomes based on race and ethnicity [7]. These disparities persist when socioeconomic and access-related factors are controlled for. The mounting evidence suggests that more than just societal racism, but institutional racism plays a role in developing these disparities.
In the United States, race and language are intricately connected. Language is a “social practice that shapes subjectivity and establishes power relations among members of different racial and class groups” [8]. English language proficiency is a less frequently considered health disparity. Language barriers increase the risk of adverse events, and patients without English proficiency are less likely to benefit from adequate communication or be involved in shared decision-making with their physicians [9].
The aim of our study was to evaluate if frequency of pain assessment, pain scores, and medication administration after cesarean delivery differed by patient race and ethnicity and primary language in women after cesarean delivery. We hypothesized that Hispanic and non-Hispanic black populations, as well as those patients with a primary language other than English, will have less frequent evaluations of their pain, report higher pain scores, and receive less pain medications than white patients.
| Materials and Methods | ▴Top |
We conducted a retrospective cohort study on all patients who had a cesarean birth at Mount Sinai South Nassau Hospital between January 1, 2018 and June 30, 2018. The study was considered exempt by the Institutional Review Board given the retrospective nature of the analyses and the evaluation of de-identified data as well as being a quality improvement study. This study was conducted in compliance with the ethical standards of the Institutional Review Board of Mount Sinai South Nassau. Mount Sinai South Nassau Hospital is a community hospital located in Oceanside, New York. There were a total of 938 women with liveborn during this time period, of whom 358 had undergone cesarean delivery. The outcomes measured included number of times pain was assessed, severe pain scores, administration of oxycodone therapeutic equivalents (OTEs) and non-steroidal anti-inflammatory drug (NSAID) doses. Patients were identified and data were extracted through the electronic medical record system.
We excluded patients who underwent cesarean hysterectomy, received general anesthesia or pain control with a patient-controlled anesthesia (PCA) device, had allergies to pain medications, and women with a known opiate addiction (n = 31) as these conditions would influence pain assessments and medication requirements. Chronic opiate use increases tolerance to these medications and has been associated with decreased pain tolerance, resulting in different pain treatment requirements that are not generalizable to the overall population [10].
A de-identified list of all women who underwent cesarean birth during the study period was obtained. Demographic and clinical information were obtained from retrospective chart review of the hospital’s electronic medical record system which contains all post-operative orders, medication administration data (type, dosing, and timing) and pain scale assessments. Clinical data obtained included parity, history of prior cesarean birth, and time and date of delivery as well as gestational age. Sociodemographic data were also obtained, including self-reported race and ethnicity, maternal age, marital status, insurance at delivery, and primary language. Race and ethnicity were categorized into five groups: non-Hispanic black, non-Hispanic white, Hispanic, Asian, and other.
During this study period, there were standardized order sets for post cesarean birth pain management that included unscheduled, as-needed NSAIDs for mild pain (characterized as a score of 1 - 3/10), unscheduled, as-needed oxycodone 5 mg/acetaminophen 325 mg every 4 h for moderate pain (score of 4 - 6), and oxycodone 10 mg/acetaminophen 650 mg every 4 h for severe pain (score of 7 - 10). In addition, obstetric providers were able to prescribe individualized analgesics (narcotic and non-narcotic) based on clinical judgement and patient-specific needs. Postpartum nursing staff performed pain assessments on patients and administered analgesic medications when requested by the patient according to these order sets.
Pain scores and medications administered after delivery were indexed to time since delivery and grouped into two discrete periods: 0 - 24 h and 25 - 48 h after delivery.
During the first 48 h from delivery, we calculated the number of pain scores recorded and whether any pain score was documented that was 7 of 10 or greater for each patient, which were considered severe scores. Women received a variety of pain medications including oxycodone, hydromorphone, codeine via both intravenous (IV) and oral (PO) routes. Each opiate dose was converted to morphine medical equivalents using a standard table. Morphine medical equivalents were further converted to 5 mg oxycodone tablet equivalents for ease of interpretation by clinicians. NSAIDs administered for pain included IV ketorolac and PO or IV ibuprofen. We quantified NSAID dose as each distinct time that NSAID medication was administered. The most common dose of NSAID in the data set was 600 mg ibuprofen and 30 mg IV ketorolac.
To evaluate whether pain management varied by patient race and ethnicity, we used statistical tests appropriate for continuous or discrete outcomes. Data for Asian and “other race” patients were combined for analysis due to low number of patients. Descriptive statistics (mean ± standard deviation or median (25th, 75th percentiles) for continuous variables; frequencies and percentages for categorical variables) were calculated for the overall sample, as well as by race/ethnicity, English/non-English speakers, and pairwise combinations of these groupings. The groups were compared using the Fisher’s exact or Chi-square test, when deemed appropriate for categorical variables. Age, body mass index (BMI), and gestational age at delivery were analyzed using the two-sample t-test (two-group comparison) and analysis of variance (three- or more-group comparison). Length of stay, number of pain assessments and severe pain scores, and OTE and NSAID doses were analyzed using the non-parametric counterparts, namely the Mann-Whitney test and the Kruskal-Wallis test. A result was considered statistically significant at the P < 0.05 level of significance. All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC).
| Results | ▴Top |
We assessed a total of 358 cesarean births during the study period (January 1, 2018 - June 30, 2018) and 327 women met the study’s inclusion criteria. Of the women who were excluded, one underwent cesarean hysterectomy, 21 were administered general anesthesia, nine used PCA or IV narcotic medications and 11 were chronic opiate users or had other contraindications to pain medications.
For the patients included, there were 3,745 discrete pain scores and 3,802 administrations of analgesic medication were analyzed. From 0 to 48 h after delivery, patients underwent a median of 11 (interquartile range 7 - 15) pain assessments and received 2,191 oxycodone tablet equivalents (interquartile range 2 - 10.5) and 1,384 doses of NSAIDs (interquartile range 2 - 6).
Comparison of baseline demographic and clinical characteristics is displayed in Table 1. Significant differences were found across race and ethnicity demonstrating a higher rate of prior c-section in the Hispanic group (58%), a trend towards older age in white and Asian/other (32.6) compared to the other groups, and lower percentages of public insurance in the Asian/other group (23.2%) versus all others. For 23.7% of the patients, their primary language was not English, in which Spanish was the primary language for 93.5% of these patients.
 Click to view | Table 1. Demographics and Clinical Characteristics |
The comparison of our study outcomes is displayed in Table 2, as well as Figures 1 and 2. The assessment and treatment of pain differed by race and ethnicity and primary language. The number of pain assessments was lowest in the Hispanic group and among non-English speaking patients. Compared with white women, Hispanic women had fewer documented pain assessments (median of 11 (8 - 16) versus median of 10 (6 - 13), P < 0.05) in the first 48 h postpartum. No difference was observed in severe pain scores by race and ethnicity or primary language.
 Click to view | Table 2. Pain Assessment, NSAID Dose, and OTE Dose by Race/Ethnicity and Primary Language |
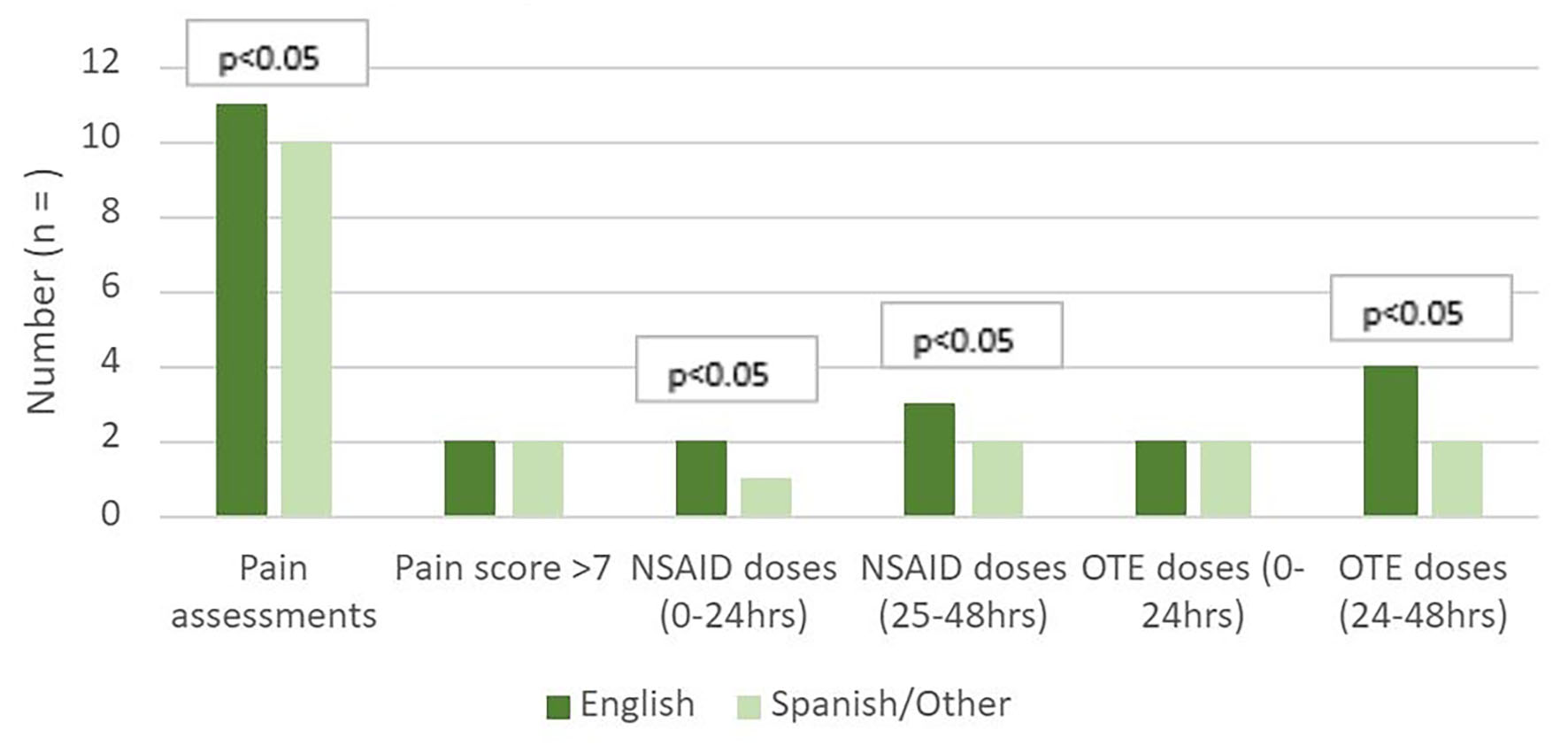 Click for large image | Figure 1. Differences in pain assessment and medications by primary language. OTE: oxycodone therapeutic equivalent; NSAID: non-steroidal anti-inflammatory drug. |
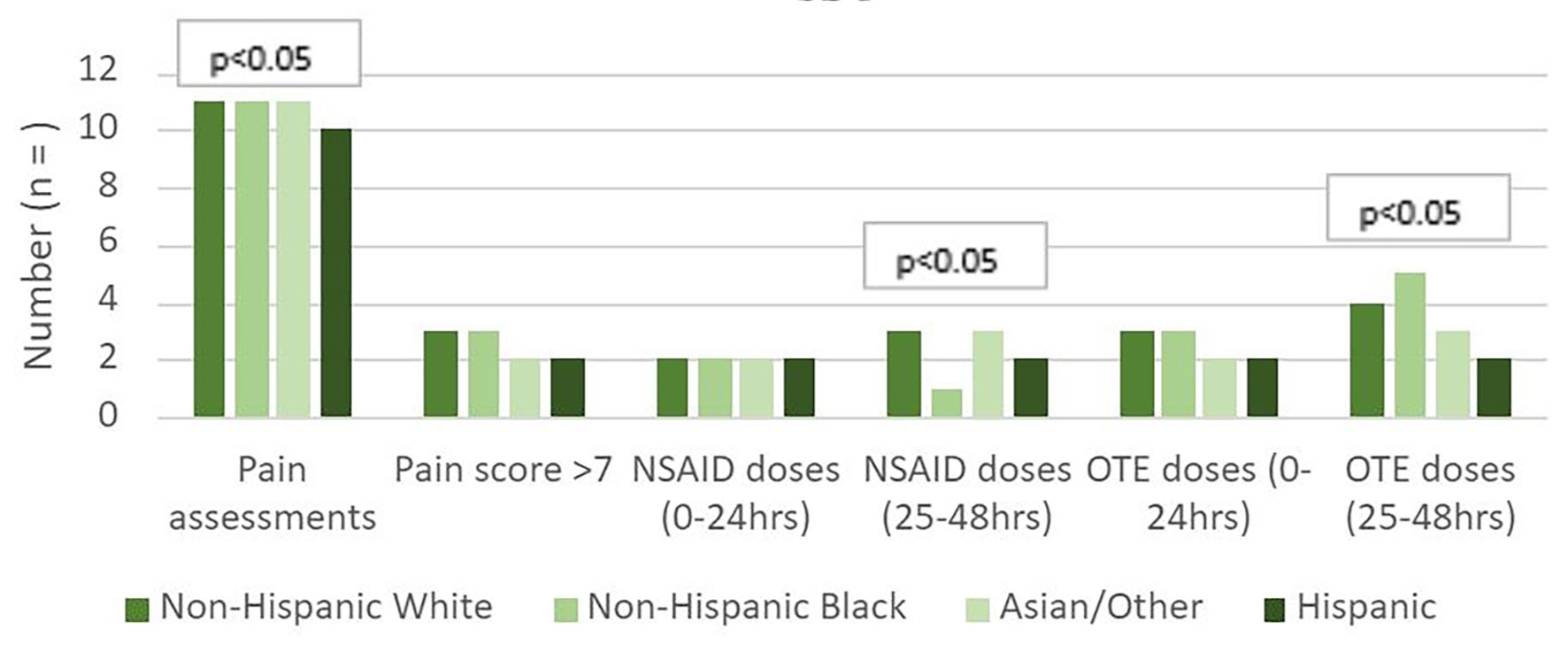 Click for large image | Figure 2. Differences in pain assessment and medications by race and ethnicity. OTE: oxycodone therapeutic equivalent; NSAID: non-steroidal anti-inflammatory drug. |
Compared with white women, black women received fewer NSAID doses (adjusted mean of 3 (1 - 4) versus 1 (1 - 2), P < 0.05) and more OTE doses (median of 4 (1 - 7) versus 5 (3 - 8)) in the 25 - 48 h postpartum. Hispanic women received fewer NSAID doses (median 2, interquartile range 1 - 4) and OTE doses (median 2, interquartile range 0 - 6) in the 25 - 58 h postpartum compared to white patients. This difference did not exist in the first 0 - 24 h postpartum. Patients whose primary language was not English received fewer NSAID doses in the 0 - 48 h and fewer OTE doses in the 25 - 48 h postpartum than their English-speaking counterparts (P < 0.03).
| Discussion | ▴Top |
Clear differences were noted in our study across racial and ethnic groups in regards to both pain assessment and medication administration, indicating that these factors continue to influence postpartum pain management. Additionally, this study found that non-English speaking patients received significantly fewer pain assessments and administration of both NSAIDs and OTE.
Disparities in pain management by race and ethnicity in the postpartum period found in this study are consistent with data from other hospitals found in recent studies [5, 6]. Although our study did not control for history of cesarean section, larger scale studies have shown these differences to persist after controlling for prior cesarean [6]. One possible explanation for the variability in pain control assessment and treatment across racial/ethnic groups is the role of implicit bias, which has been shown to influence how providers treat pain across racial groups in other settings, such as treatment of pain in cancer patients [11]. Interestingly, our study demonstrated that non-Hispanic black women received more OTE rather than NSAIDs and may be secondary to implicit bias. Although not expressly investigated in this study, many studies in the past have looked at implicit biases held by healthcare providers. These studies have primarily focused on implicit biases pertaining to race and ethnicity, and have shown that these biases are pervasive throughout healthcare across different professions, including physicians and nurses [12]. Although causation can be difficult to prove, and few studies have investigated the association of implicit bias with patient outcomes, multiple studies have found that higher levels of implicit bias are associated with worse patient-physician interactions [13]. Implicit bias pertaining to race and ethnicity has also been correlated with differences in decisions regarding as well as adherence to treatment, and some studies have found differences in patient health outcomes [14].
Additionally, we demonstrated that non-English speaking patients received fewer pain assessments as well as fewer NSAID and OTE doses which may indicate language as a barrier for equitable pain management in the postpartum period. Language is a complex system of communication that is deeply rooted in culture and heritage, and linguistic barriers have been found to impair communication across cultures [15]. Our study adds to the data suggesting language as a barrier to equal care.
We were able to use readily available data regarding pain assessments and scoring in our hospital’s electronic medical record system to identify areas where disparities exist. Prior to the study pain assessments are made at the time of vitals being taken and at the discretion of nurses or patient request which are not standardized. Potential ways to relieve this disparity include standardized pain medication administration systems and scheduled pain assessments. The American College of Obstetricians and Gynecologists recommends the use of standardized multi-modal pain management with around-the-clock non-opioid medication administration [16]. This standardization may help reduce or eliminate these disparities and should be further investigated. Further investigations should also include the overt role of implicit bias in postpartum pain management.
Despite these findings, limitations to our study include inability to directly assess patient and provider factors. Our study did not assess patient’s beliefs about pain tolerance and pain expression, nor any beliefs or potential biases among healthcare providers related to the expression of pain. Additionally, this study occurred at a single institution that may not be generalizable to other populations.
Conclusions
Our study contributes to the growing body of evidence that inequities in pain control assessment and treatment exist, not only among various races and ethnicities, but also with regards to primary language. These findings are consistent with prior work in this area, but also extend these disparities to populations with limited English. The root cause of this disparity requires further investigation. One possible future direction is investigation into how the integration of standardized multi-modal pain management may or may not reduce disparities in pain assessment and treatment.
Acknowledgments
None to declare.
Financial Disclosure
This research project did not receive any grants or other financial support.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
Alison Wiles conceived and designed the project, collected data, performed analysis and wrote the paper. Electra Korn conceived and designed the project, collected data, and wrote the paper. Cheryl Dinglas performed analysis and edited the paper. Beth Bentley and Jonathan Rosner collected data and performed analysis. Salma Rahimi oversaw the project and manuscript writeup.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Smedley BD, Stith AY, Nelson AR. Institute of Medicine (US) Committee on understanding and eliminating racial and ethnic disparities in health care. Unequal treatment: Confronting racial and ethnic disparities in health care. 2003.
- Shah AA, Zogg CK, Zafar SN, Schneider EB, Cooper LA, Chapital AB, Peterson SM, et al. Analgesic access for acute abdominal pain in the emergency department among racial/ethnic minority patients: a nationwide examination. Med Care. 2015;53(12):1000-1009.
doi pubmed - Ly DP. Racial and ethnic disparities in the evaluation and management of pain in the outpatient setting, 2006-2015. Pain Med. 2019;20(2):223-232.
doi pubmed - Lange EMS, Rao S, Toledo P. Racial and ethnic disparities in obstetric anesthesia. Semin Perinatol. 2017;41(5):293-298.
doi pubmed - Johnson JD, Asiodu IV, McKenzie CP, Tucker C, Tully KP, Bryant K, Verbiest S, et al. Racial and ethnic inequities in postpartum pain evaluation and management. Obstet Gynecol. 2019;134(6):1155-1162.
doi pubmed - Badreldin N, Grobman WA, Yee LM. Racial disparities in postpartum pain management. Obstet Gynecol. 2019;134(6):1147-1153.
doi pubmed - Grobman WA, Bailit JL, Rice MM, Wapner RJ, Reddy UM, Varner MW, Thorp JM, Jr., et al. Racial and ethnic disparities in maternal morbidity and obstetric care. Obstet Gynecol. 2015;125(6):1460-1467.
doi pubmed - Parmegiani A, Holliday A, Hyde M, Kullman J, Ricento T, Ramirez J, et al. On race, language, power and identity: Understanding the intricacies through multicultural communication, language policies, and the ebonics debate. TESOL Q. 2006;4(3):641-648.
doi - Ferguson WJ, Candib LM. Culture, language, and the doctor-patient relationship. Fam Med. 2002;34(5):353-361.
- Alford DP, Compton P, Samet JH. Acute pain management for patients receiving maintenance methadone or buprenorphine therapy. Ann Intern Med. 2006;144(2):127-134.
doi pubmed - Fiscella K, Epstein RM, Griggs JJ, Marshall MM, Shields CG. Is physician implicit bias associated with differences in care by patient race for metastatic cancer-related pain? PLoS One. 2021;16(10):e0257794.
doi pubmed - FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19.
doi pubmed - Maina IW, Belton TD, Ginzberg S, Singh A, Johnson TJ. A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Soc Sci Med. 2018;199:219-229.
doi pubmed - Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, Eng E, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105(12):e60-76.
doi pubmed - Schouten BC, Meeuwesen L. Cultural differences in medical communication: a review of the literature. Patient Educ Couns. 2006;64(1-3):21-34.
doi pubmed - American College of Obstetricians Gynecologists' Committee on Clinical, Consensus-Obstetrics. Pharmacologic stepwise multimodal approach for postpartum pain management: ACOG clinical consensus No. 1. Obstet Gynecol. 2021;138(3):507-517.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
