| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Original Article
Volume 11, Number 2, June 2022, pages 33-38
Risk Factors for Intrapartum Fever of Infectious Origin and Maternal and Neonatal Morbidity
Maitane Zubikaraia, c, Sandra Huertaa, Carla BlascoDeImaza, Ane Mujikab, Nerea Marina, b, Jose Angel Navarrinaa, b, Arantza Lekuonaa, b
aDepartment of Obstetrics and Gynecology, Donostia University Hospital, San Sebastian, Spain
bDepartment of Medical-Surgical Specialties, University of the Basque Country, Leioa, Spain
cCorresponding Author: Maitane Zubikarai, Department of Obstetrics and Gynecology, Donostia University Hospital, San Sebastian, Spain
Manuscript submitted January 31, 2022, accepted March 31, 2022, published online April 12, 2022
Short title: Infectious Intrapartum Fever and Morbidity
doi: https://doi.org/10.14740/jcgo794
| Abstract | ▴Top |
Background: Intrapartum fever defined as temperature ≥ 38 °C occurs in 1.6-14.6% of pregnancies and may be caused by an infectious or inflammatory process. The aim of this study was to analyze the possible risk factors and the neonatal and maternal morbidity-mortality in both cases.
Methods: This was a retrospective cohort study, including full-term singleton cephalic presentation pregnant women who gave birth in the Donostia University Hospital during 2017 - 2018 and developed fever ≥ 38 °C. Infectious intrapartum fever was classified by the presence of positive urine, blood or placenta culture or pathological placenta while fever of inflammatory etiology was classified by negative cultures.
Results: Women over 32 years of age (odds ratio (OR): 3.07, 95% confidence interval (CI): 1.35 - 7) and those with labor duration between fever presentation to delivery > 6 h (OR: 6.11, 95% CI: 1.35 - 27.62) had a statistically significant increased risk of presenting fever of infectious origin. There were no statistically significant differences between the two groups regarding maternal and neonatal morbidity and mortality.
Conclusions: This study found a significant association between maternal age > 32 years old and labor duration > 6 h from fever onset to birth and a higher risk of maternal infectious fever.
Keywords: Intrapartum fever; Infection; Inflammatory; Risk factors; Neonate; Morbidity
| Introduction | ▴Top |
Intrapartum fever is a heterogeneous condition and new terms have been proposed to classify intrauterine inflammation, infection, or both (triple I). Isolated maternal fever is defined as oral temperature of 39.0 °C or greater on one occasion or temperature between 38 °C and 39 °C in two temperature measures repeated at 30 min. Suspected triple I is considered fever in addition to any of the following: fetal tachycardia, maternal white blood cell count greater than 15,000 per mm3 or purulent fluid from the cervical os. Confirmed triple I includes amniocentesis-proven infection with a positive Gram stain, low glucose or positive amniotic fluid culture or placental histologic infection [1, 2].
The prevalence of intrapartum fever in term deliveries ranges from 1.6% to 14.7% [3-5].
Several studies have demonstrated the association between fever during labor and adverse maternal and neonatal outcomes [6]. However, others have described that adverse results are related to medical interventions associated with fever, and not strictly to fever [5].
Fever can be caused by an inflammatory process or an infection [7]. Different possible risk factors have been established for both processes, such as epidural analgesia [8-10] and prolonged rupture of membranes [5], respectively.
Therefore, the objective of this study was to analyze the characteristics of patients with infectious and inflammatory intrapartum fever at the Donostia University Hospital in order to identify the risk factors related to each group. Furthermore, the secondary aim was to investigate maternal and neonatal outcomes following intrapartum fever by infection or inflammation.
| Materials and Methods | ▴Top |
This was a retrospective cohort study performed between January 2017 and December 2018 in the Donostia University Hospital, which is a tertiary care center for obstetrics and neonates. The study group included pregnant women at term (37 - 42 weeks) who developed systemic fever ≥ 38 °C during labor.
Eligibility criteria were singleton gestation at term, cephalic presentation, no fetal anomalies, and fever ≥ 38 °C during labor.
The exclusion criteria were maternal fever on admission, multiple pregnancy, preterm birth, known fetal chromosomal or structural anomalies, stillbirths and elective cesarean delivery.
According to our protocols, blood and urine cultures were taken and antipyretic and antibiotic treatment was established (ampicillin 2 g every 6 h and gentamicin 1.5 mg/kg every 8 h) in patients who developed intrapartum fever (≥ 38 °C). Following delivery, placental cultures were taken, and placental anatomy and pathology studies were performed.
The maternal demographic and obstetrical data collected included age, previous vaginal deliveries, history of cesarean delivery, gestational age and associated maternal morbidity (diabetes mellitus, preeclampsia, hypothyroidism, anemia, etc.).
The possible intrapartum risk factors recorded were induction of labor, type of induction, epidural anesthesia, number of vaginal examinations, internal catheter placement (dynamic or fetal heart rate), group B streptococcus (GBS) culture, time from rupture of membranes to labor onset (minutes), time from rupture of membranes to fever (minutes), time from fever onset to delivery (minutes) and length of stay in the labor area (minutes).
A subgroup of infectious intrapartum fever was diagnosed by the presence of a positive urine, blood, or placenta culture and placental histopathologic infection. Histologic infection was defined by the presence of acute histologic changes of the amniotic membrane and placenta characterized by polymorphonuclear leukocyte infiltration.
The neonatal outcomes evaluated were intrapartum fetal tachycardia, umbilical artery cord pH, birth weight, first minute Apgar score, fifth minute Apgar score, admission to neonatal intensive care unit (NICU), diagnosis for admission, culture results and need for antibiotic therapy. The maternal outcome recorded was the current mode of delivery.
Obstetric and medical history, labor and delivery data, including neonatal and maternal outcomes were collected from the electronic medical history.
The statistical analyses were performed using the SPSS program. Continuous variables were described as mean and standard deviation and categorical variables as rate. The Fisher’s and Chi-square tests were used for comparing categorical variables and the Student’s t-test was used for continuous variables. A P-value of ≤ 0.05 was considered statistically significant. Multiple logistic regression was used to investigate independent associations between infectious intrapartum fever and the variables described above.
The study was approved by the Clinical Investigation Ethics Committee of the Donostia University Hospital (10/2019). This study was conducted in compliance with all the applicable institutional ethical guidelines.
| Results | ▴Top |
Among 6,926 pregnancies in the Donostia University Hospital, a total of 203 patients were included in the study group (Fig. 1).
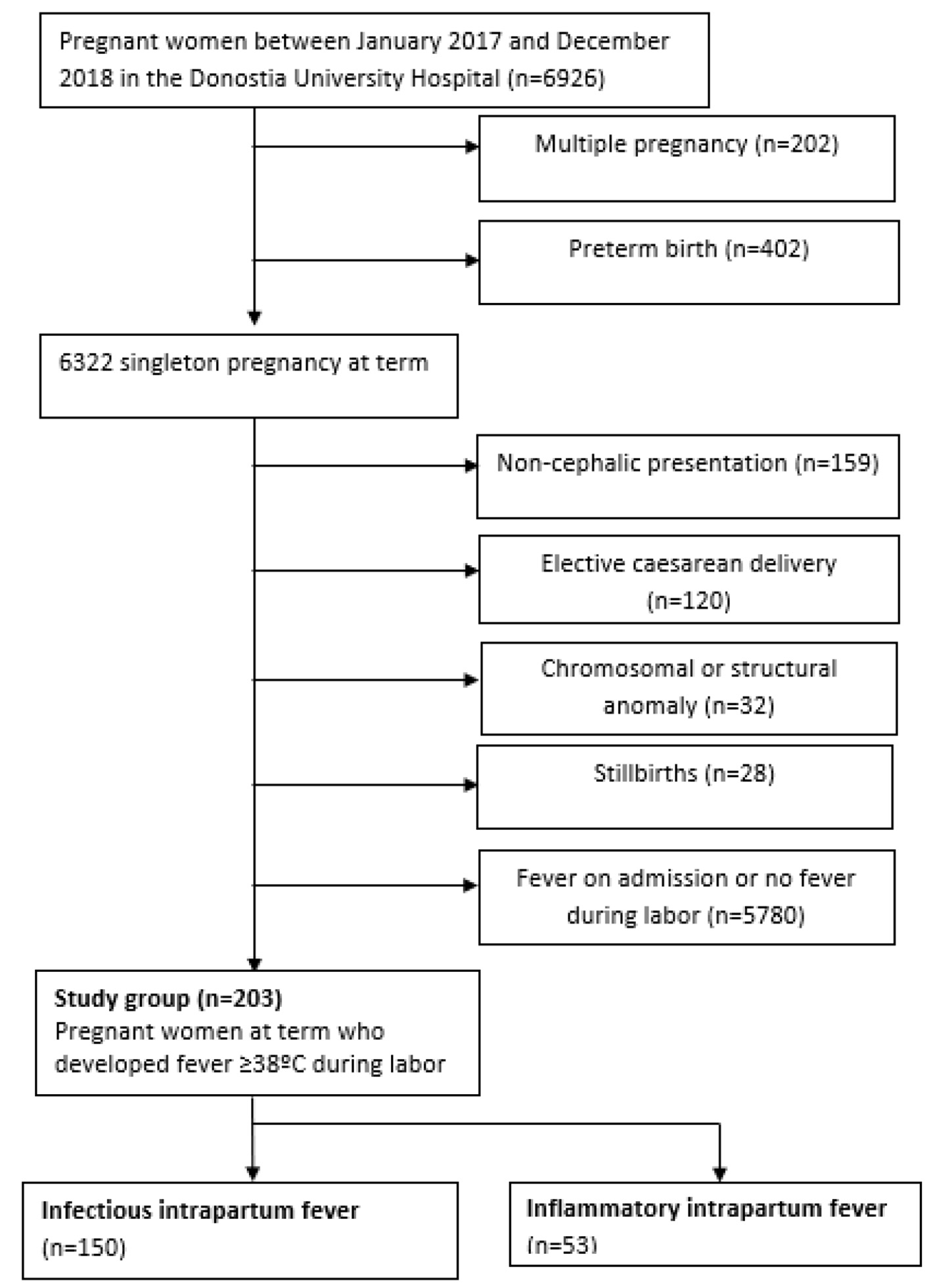 Click for large image | Figure 1. Flow chart of the study group. |
The incidence of intrapartum fever was 2.93%.
The maternal and neonatal characteristics of the pregnancies developing intrapartum fever are shown in Table 1.
 Click to view | Table 1. Maternal and Neonatal Demographic Data of Women Who Developed Intrapartum Fever During 2017 - 2018 |
Table 2 shows the comparison of the risk factors of the maternal inflammatory and infectious intrapartum fever subgroups. Maternal age > 32 years was associated with infectious intrapartum fever (odds ratio (OR): 3.07; 95% confidence interval (CI): 1.35 - 7).
 Click to view | Table 2. Risk Factors for Maternal Infectious Intrapartum Fever |
There were no differences in other demographic and obstetric features, such as nulliparity, gestational age or previous cesarean section.
Regarding labor and delivery characteristics, pregnant women who developed infectious intrapartum fever presented a significantly longer period (> 6 h) between fever onset and delivery (OR: 6.11; 95% CI: 1.35 - 27.62).
Induction of labor, internal catheter use, and the number of vaginal examinations did not differ between groups.
Neonatal outcomes were similar, with no differences between the infectious and inflammatory intrapartum fever groups in relation to the Apgar test, umbilical artery cord pH and NICU admission (Table 3). The rates of cesarean delivery and normal delivery were the same in both groups.
 Click to view | Table 3. Maternal and Neonatal Outcomes of Maternal Infectious Intrapartum Fever |
The most frequent microorganisms found in infectious intrapartum fever cultures were Escherichia coli (18.7%) followed by Streptococcus agalactiae (4.4%) and Enterococcus faecalis (3.4%) (Fig. 2).
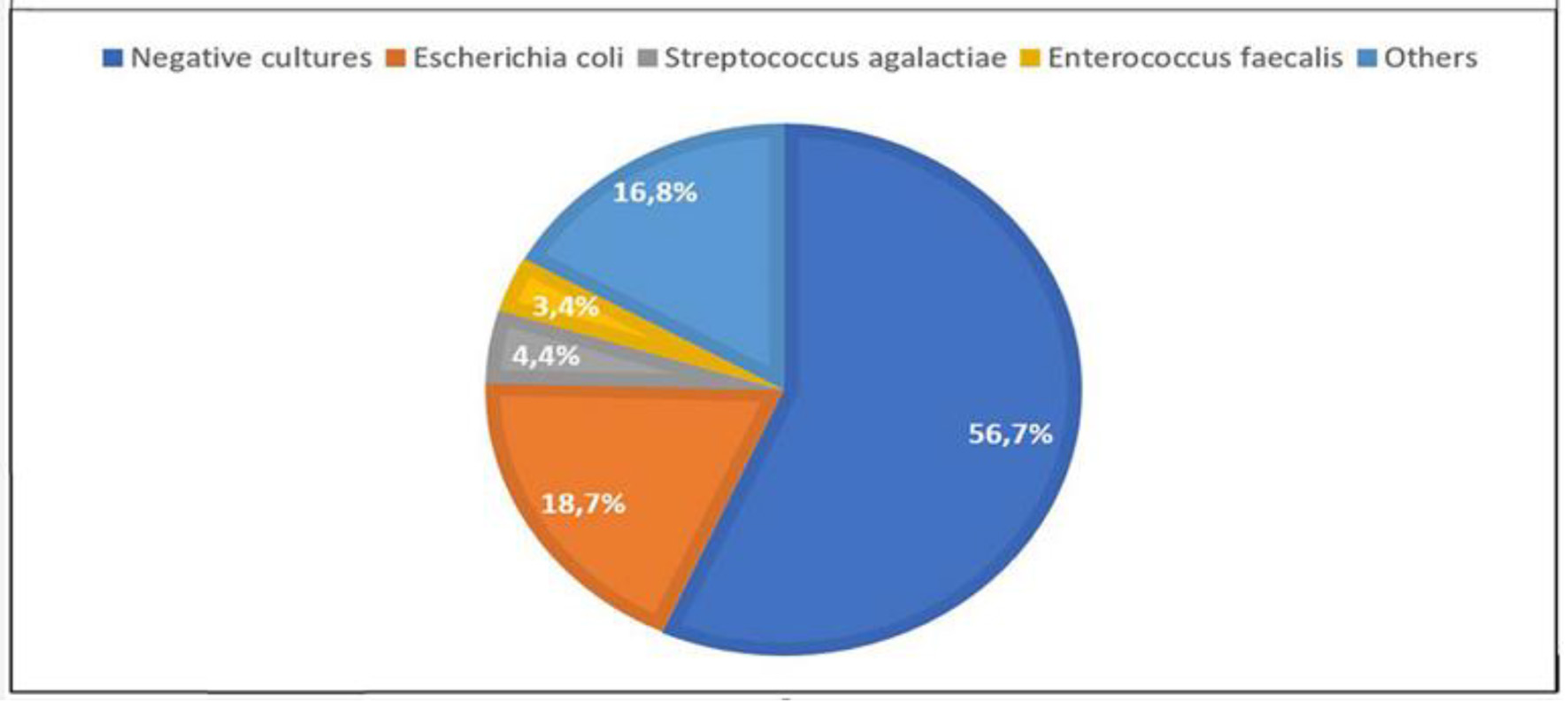 Click for large image | Figure 2. Microorganism culture results for maternal infectious intrapartum fever. |
| Discussion | ▴Top |
The incidence of maternal intrapartum fever in the present study was 2.93%. This rate varies among studies, ranging from 1.3% to 14.7% [3, 6, 11]. While our findings agree with those of other studies, temperature measurement for the diagnosis of “triple I” did not follow the criteria of Higgins et al [1].
Curtin et al [12] and Maayan-Metzger et al [5] demonstrated that epidural analgesia is independently associated with intrapartum fever. Similar to the studies carried out by Ashwal et al [3] and Towers et al [6], the cases of infectious intrapartum fever in our study were not associated with epidural anesthesia as a risk factor (P = 0.551). This result is consistent with the theory of maternal hyperthermia induced by epidural analgesia in intrapartum fever suggested by Goetzl [13] and Sharpe et al [10].
According to Kovo et al [14], multiple vaginal examinations are related to a higher risk of intrapartum fever and placental inflammatory findings of chorioamnionitis origin. Nevertheless, our study found no association between the number of vaginal examinations and the development of infectious intrapartum fever, probably due to the small study population.
In our study, a time > 6 h between intrapartum fever onset and delivery was more likely to be associated with the presentation of infectious intrapartum fever. Herbst et al [15] reported a strong linear association between the duration of rupture of membranes and neonatal septicemia. Our findings agree with the association between a longer duration to delivery and the infectious causality but not with adverse neonatal outcomes.
The microorganisms determined to be involved in the development of intrapartum fever of infectious origin in the present study were similar to those described in the study by Apantaku and Mulik [8].
Maayan-Metzger et al [5] and Lieberman et al [9] described higher rates of cesarean section and instrumental deliveries in women developing intrapartum fever. However, other studies reporting intrapartum fever of infectious origin [3] did not detect maternal complications in the group of intrapartum fever with positive cultures, coinciding with our findings of no differences in the mode of delivery.
Neonatal outcomes were similar in both groups of intrapartum fever, in contrast to the findings of Lieberman et al [16], Burgess et al [17] and Ashwal et al [3] who reported a higher rate of adverse outcomes in maternal intrapartum fever and specially in infectious fever. The differences between the results of the present study and those of the previous authors are likely related to the small sample size of our study.
The limitations of this investigation are the retrospective design and the relatively small population of the two groups compared. Despite this, the study has several strengths; the information was collected from a tertiary care center for obstetrics and neonates and the data are based on daily clinical practice following the same protocols.
In conclusion, infectious intrapartum fever is associated with age > 32 years and a > 6 h duration between fever onset and delivery. Nevertheless, no association was found between infectious intrapartum fever and adverse maternal and neonatal outcomes. Hence, the unfavorable outcomes seem be related to maternal hyperthermia condition.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
All participants provided signed informed consent.
Author Contributions
MZ contributed to designing the work, the analysis and interpretation of data and writing the manuscript. Both SH and CBDI contributed to data acquisition and analysis. AM contributed to data acquisition and analysis. NM contributed to the conception of the study, interpretation of data, provided critical revision to the manuscript and gave the final approval. Both JAN and AL provided critical revision and approval of the manuscript to be published.
Data Availability
The data supporting the findings of this study are available from the corresponding author.
| References | ▴Top |
- Higgins RD, Saade G, Polin RA, Grobman WA, Buhimschi IA, Watterberg K, Silver RM, et al. Evaluation and management of women and newborns with a maternal diagnosis of chorioamnionitis: summary of a workshop. Obstet Gynecol. 2016;127(3):426-436.
doi pubmed - Committee Opinion No. 712: Intrapartum Management of Intraamniotic Infection. Obstet Gynecol. 2017;130(2):e95-e101.
doi pubmed - Ashwal E, Salman L, Tzur Y, Aviram A, Ben-Mayor Bashi T, Yogev Y, Hiersch L. Intrapartum fever and the risk for perinatal complications - the effect of fever duration and positive cultures. J Matern Fetal Neonatal Med. 2018;31(11):1418-1425.
doi pubmed - Lieberman E, Lang J, Richardson DK, Frigoletto FD, Heffner LJ, Cohen A. Intrapartum maternal fever and neonatal outcome. Pediatrics. 2000;105(1 Pt 1):8-13.
doi pubmed - Maayan-Metzger A, Mazkereth R, Shani A, Kuint J. Risk factors for maternal intrapartum fever and short-term neonatal outcome. Fetal Pediatr Pathol. 2006;25(3):169-177.
doi pubmed - Towers CV, Yates A, Zite N, Smith C, Chernicky L, Howard B. Incidence of fever in labor and risk of neonatal sepsis. Am J Obstet Gynecol. 2017;216(6):596 e591-596 e595.
doi pubmed - Romero R, Chaemsaithong P, Korzeniewski SJ, Kusanovic JP, Docheva N, Martinez-Varea A, Ahmed AI, et al. Clinical chorioamnionitis at term III: how well do clinical criteria perform in the identification of proven intra-amniotic infection? J Perinat Med. 2016;44(1):23-32.
- Apantaku O, Mulik V. Maternal intra-partum fever. J Obstet Gynaecol. 2007;27(1):12-15.
doi pubmed - Lieberman E, Cohen A, Lang J, Frigoletto F, Goetzl L. Maternal intrapartum temperature elevation as a risk factor for cesarean delivery and assisted vaginal delivery. Am J Public Health. 1999;89(4):506-510.
doi pubmed - Sharpe EE, Arendt KW. Epidural labor analgesia and maternal fever. Clin Obstet Gynecol. 2017;60(2):365-374.
doi pubmed - San Roman MV, Lobato JL, Valladolid A, Fernandez MJ, Fraca M, Lopez M. La fiebre intraparto como factor predictivo de parto distocico y resultado neonatal adverso. Clínica e Investigacion en Ginecologia y Obstetricia. 2015;42(4):171-173.
doi - Curtin WM, Katzman PJ, Florescue H, Metlay LA, Ural SH. Intrapartum fever, epidural analgesia and histologic chorioamnionitis. J Perinatol. 2015;35(6):396-400.
doi pubmed - Goetzl L. Epidural analgesia and maternal fever: a clinical and research update. Curr Opin Anaesthesiol. 2012;25(3):292-299.
doi pubmed - Kovo M, Schreiber L, Ben-Haroush A, Shor S, Golan A, Bar J. Intrapartum fever at term: clinical characteristics and placental pathology. J Matern Fetal Neonatal Med. 2012;25(8):1273-1277.
doi pubmed - Herbst A, Kallen K. Time between membrane rupture and delivery and septicemia in term neonates. Obstet Gynecol. 2007;110(3):612-618.
doi pubmed - Lieberman E, Eichenwald E, Mathur G, Richardson D, Heffner L, Cohen A. Intrapartum fever and unexplained seizures in term infants. Pediatrics. 2000;106(5):983-988.
doi pubmed - Burgess APH, Katz JE, Moretti M, Lakhi N. Risk factors for intrapartum fever in term gestations and associated maternal and neonatal sequelae. Gynecol Obstet Invest. 2017;82(5):508-516.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
