| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Case Report
Volume 13, Number 2, June 2024, pages 41-47
Condyloma Lata: A Vulvar Manifestation of Secondary Syphilis
Esther Patricia Escamilla Galindoa, c, Elisabet Barahona San Millana, Salvador Nauzet Del Rosario Lorenzoa, Janed Lourdes Santana Mateoa, Norberto Fidel Medina Ramosa, Francisco Granados Pachecob, Alicia Inmaculada Martin Martineza
aDepartment of Gynecology and Obstetrics, Hospital Complex Materno-Infantil of Gran Canaria, Las Palmas de Gran Canaria, Spain
bPathology Department, Hospital Complex Materno-Infantil of Gran Canaria, Las Palmas de Gran Canaria, Spain
cCorresponding Author: Esther Patricia Galindo Escamilla, Department of Gynecology and Obstetrics, Hospital Complex Materno-Infantil of Gran Canaria, Las Palmas de Gran Canaria, Spain
Manuscript submitted March 2, 2024, accepted April 11, 2024, published online June 30, 2024
Short title: Secondary Syphilis Arising as Condyloma Lata
doi: https://doi.org/10.14740/jcgo960
| Abstract | ▴Top |
In the initial decades of the 21st century, a rise in the incidence of syphilis has been observed in all developed countries. This disease has become not only a public health concern, but also a problem in clinical practice, since clinicians need to have sufficient knowledge and experience for an early diagnosis and treatment. Syphilis is a sexually transmitted infection caused by the spirochete bacterium Treponema pallidum. In secondary syphilis, condyloma lata, a papular lesion typical of this stage of the disease, has been reported in 6% to 23% of patients. Here we present two cases of patients diagnosed with secondary syphilis, who presented condyloma lata on the vulvar area as the first clinical manifestation. Biopsy of lesions and observation with dark-field microscopy revealed abundant spirochetes. It was not an easy diagnosis either for the clinician and the pathologist as it can be similar to other dermatological conditions, such as anogenital warts (condyloma acuminata). Patients were treated with penicillin until complete resolution of the clinical signs. Secondary syphilis is currently uncommon in developed countries, especially with condyloma lata as the first clinical manifestation.
Keywords: Secondary syphilis; Condyloma lata; Sexually transmitted infection
| Introduction | ▴Top |
Syphilis is a sexually transmitted infection caused by the spirochete bacterium Treponema pallidum. Transmission can occur through sexual contact via skin lesions, or vertically through the placenta/birth canal via genital lesions if present, resulting in congenital syphilis. The infection can infrequently be acquired via non-sexual interactions, such as skin-to-skin, or via blood transfer [1]. Syphilis is a chronic disease with an undulating course; the early form is classified as primary, secondary and early latent, and late syphilis that includes late latent and tertiary syphilis [2, 3]. According to the Center of Disease Control, syphilis case reports continue to increase since reaching a historic low in 2000 and 2001. During 2021, there were 176,713 new cases of syphilis (all stages) [4]. Nevertheless, the incidence of this disease is underestimated because some countries do not report all cases or report them with significant delays [5]. Secondary syphilis is the most recognized clinical syndrome of syphilis. Symptoms that may precede or coincide with secondary syphilis are malaise, myalgia, odynophagia, headache, or low-grade fever 3 to 12 weeks after resolution of the chancre or even at the same time. These manifestations are due to hematogenous spread of spirochetes [6].
The symptoms include a non-pruritic rash, usually on the palms of the hands and soles of the feet; white or grey lesions also appear in moist areas, such as the creases, groin, lips or anus [6], most often accompanied by generalized lymphadenopathy [7]. It should be mentioned that the symptoms disappear without treatment [8]. Mucocutaneous lesions associated to secondary syphilis usually appear on the anogenital region as flat reddish-brown or purple lesions called condyloma lata [9].
In the first few years of the 21st century, a rise in the incidence of syphilis has been observed in all developed countries. This disease has become not only a public health concern, but also a problem in clinical practice, since practitioners need to have sufficient knowledge and experience for an early diagnosis and treatment [10, 11]. According to Spanish epidemiological surveillance data, the number of cases in Spain increased to 14 per 100,000 people, in 2021 [12].
Here we present two cases of vulvar condyloma lata as a manifestation of Treponema pallidum infection in its secondary stage.
| Case Reports | ▴Top |
Case 1
Investigations
A 42-year-old patient with no related medical background, former user of crack, cocaine and marijuana, who had undergone a drug rehabilitation treatment, and reported having engaged in high-risk sexual practices with multiple partners in the past, presented at the emergency room with a 1-week history of bilateral highly painful raised vulvar lesions. Physical examination revealed well-defined bilateral papules of irregular surface, tender to palpation, and reactive bilateral inguinal lymphadenopathy. No further associated systemic signs or skin abnormalities were found. The patient was initially diagnosed with herpes simplex and prescribed valaciclovir plus topical anesthetics. Three days later, the lesions had significantly increased in size, covering the labia majora and minora, as well as a portion of the perianal region. The patient’s main complaint was of genital pain. She was prescribed topical corticosteroids and referred to the Lower Genital Tract Pathology Unit (LGTPU).
In the LGTPU, thorough examination of the genital area and the entire body surface was conducted. Despite being under the prescribed corticosteroid therapy, the patient’s condition had not improved. Examination revealed exophytic lesions on the labia majora and bilateral non-painful inguinal lymphadenopathies (Fig. 1). The lesions were irregularly shaped, with the largest one being approximately 4 cm in length, located on the left side. No abnormal colposcopy findings were detected in the vagina or the cervix. Thorough inspection of the skin on both the upper and lower limbs showed maculopapular lesions without pruritus.
 Click for large image | Figure 1. Condyloma lata at presentation (case 1). |
Diagnosis
Vaginal and endocervical swabs were collected, as well as a biopsy specimen from the largest lesion, and serological tests for hepatitis A, B, C, human immunodeficiency virus (HIV) and Treponema pallidum were requested, even if vulvar lesion aspect was atypical.
The histological study showed marked pseudoepitheliomatous hyperplasia with regular acanthosis at the periphery and a polymorphonuclear infiltrate in the upper layers. Subepithelial examination revealed an inflammatory infiltrate rich in plasma cells, and frequent vasculitis images (Fig. 2). No fungal structures were found with periodic acid-Schiff stain. The diagnosis of condyloma lata was confirmed by using an anti-treponemal technique, which showed numerous spirochetes in the basal layers of the hyperplastic epithelium. Neisseria gonorrhoeae and Trichomonas vaginalis were isolated from the vaginal and endocervical swabs. Serological tests were negative for hepatitis and HIV, though the treponemal test was positive with a rapid plasma reagin (RPR) titer of 1:4.
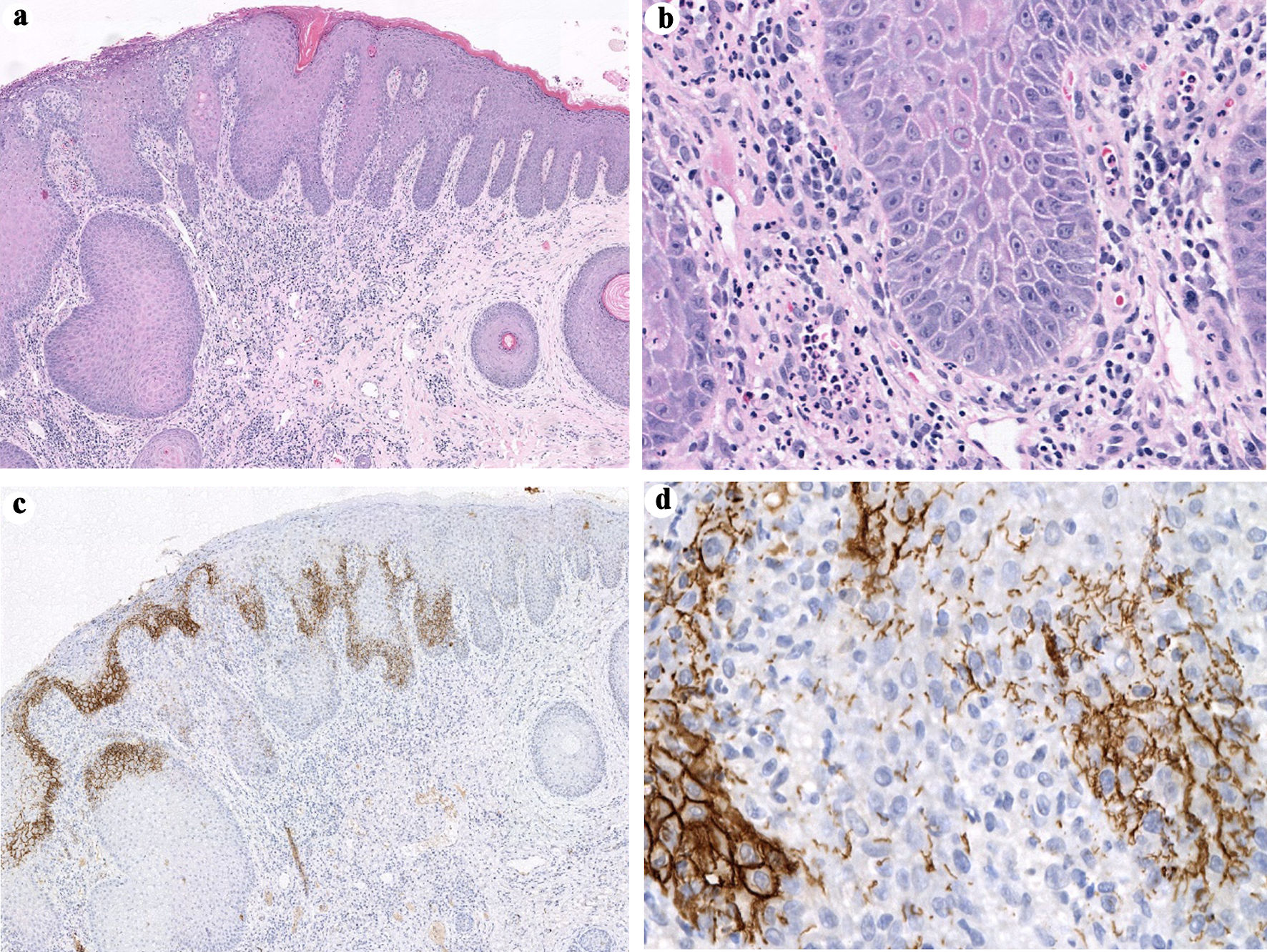 Click for large image | Figure 2. Histopathology of condyloma lata. (a) and Hematoxylin & eosin stain shows intense pseudoepitheliomatous hyperplasia with regular acanthosis at the periphery and a polymorphonuclear infiltrate in the upper layers. (b) Subepithelial examination revealed inflammatory infiltration rich in plasma cells, as well as frequent vasculitis images. (c, d) Treponema immunohistochemistry. The spirochaetes are predominantly arranged in a basal distribution. |
Treatment
Upon consultation, clinicians from the Infectious Diseases Unit (IDU) proposed the following therapeutic regimen: a single dose of intramuscular ceftriaxone 250 mg, three doses of intramuscular penicillin G benzathine 2.4 million IU, and oral administration of metronidazole 500 mg, every 12 h for 7 days.
Follow-up and outcomes
After 7 days of treatment, the patient reported feeling much better, the vulvar lesions were markedly reduced, with no associated pruritus or pain, and the palm/sole skin lesions had also improved, although the non-painful bilateral inguinal lymphadenopathies persisted (Fig. 3). The correct response to treatment confirmed that she was cured with follow-up 6, 12, and 24 months after treatment with a clinical evaluation and serial non-treponemal (Venereal Disease Research Laboratory (VDRL) and RPR) testing.
 Click for large image | Figure 3. Lesions after treatment with penicillin G benzathine 2.4 million IU (case 1). |
Case 2
Investigations
A 35-year-old woman presented to us with a history of intravenous heroin use, smoking over 20 cigarettes per day since adolescence, and using marijuana since the age of 20. She reported having a long-term, stable sexual partner with whom she had unprotected sex. The patient presented to the Gynecological Emergency Department with vulvar pruritus, dryness, and multiple painful raised vulvar lesions (Fig. 4). The symptoms had appeared 12 days before and worsened in the last 48 h. Additionally, she reported a maculopapular rash affecting the entire body surface, including the palms, soles, and oral mucosa. There were no further associated symptoms.
 Click for large image | Figure 4. Condyloma lata at presentation (case 2). |
Diagnosis
Physical examination showed several rounded papules on the trunk and the limbs with palm/sole involvement. Additionally, two ulcerated lesions of approximately 2 cm were found on the oral mucosa. Genital examination showed multiple raised lesions 1 - 2 cm in diameter on the vulva, along with tender bilateral inguinal lymphadenopathies. Blood samples were collected for serological test of syphilis, HIV and hepatitis A, B, and C. Results were negative for hepatitis and HIV, while the treponemal test was positive with an RPR titer of 1:64. Endocervical, vaginal and oral swabs were also collected for histological examination, which revealed the presence of spirochetes (Fig. 5).
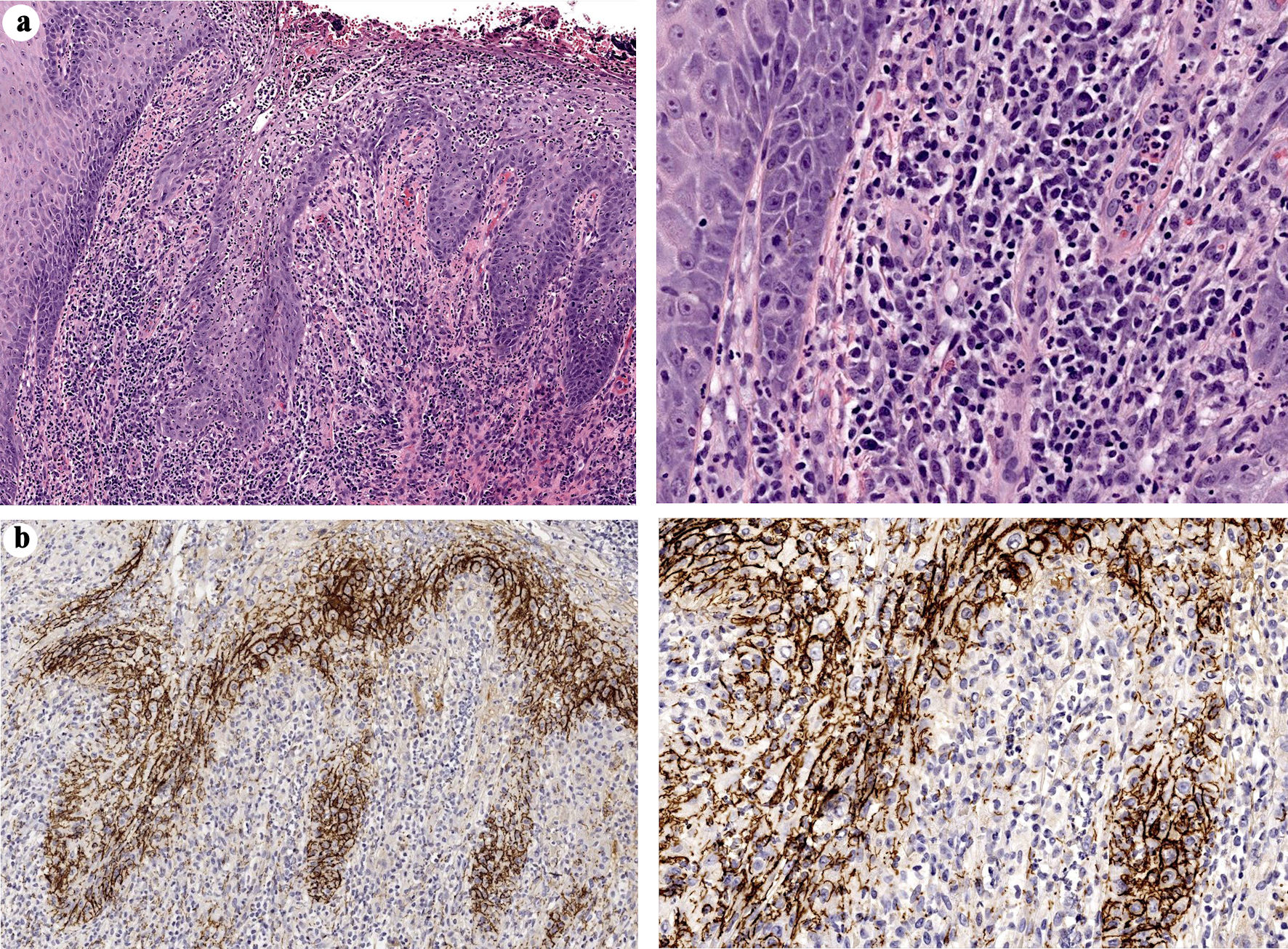 Click for large image | Figure 5. Histopathology of condyloma lata (case 2). (a) Hematoxylin & eosin stain shows epidermal hyperplasia and a dense mixed inflammatory infiltrate with abundant plasma cells. (b) Positive immunohistochemical staining for Treponema was observed. |
Treatment
The patient was administered an initial dose of intramuscular penicillin G benzathine (2.4 million IU) and referred to the LGTPU and the IDU for management of the disease. In a follow-up visit 7 days after initiating the treatment, she reported that she had experienced relief of the pruritus within the first 24 h from penicillin administration. Furthermore, a physical examination showed that the lymphadenopathies had disappeared, and the lesions had improved noticeably. She received a second penicillin dose and was scheduled to receive the final dose 7 days later.
Follow-up and outcomes
After 15 days of treatment, the vulvar and oral lesions had completely disappeared, and the maculopapular rash had almost resolved. Three months after the acute infection, serological tests showed that there was no coinfection with HIV and the treponemal test RPR titer was 1:4.
| Discussion | ▴Top |
Syphilis is typically diagnosed by serology, but a diagnosis can also be confirmed by immunohistopathology or nucleic acid amplification if biopsy of a lesion is obtained [13].
Secondary syphilis is characterized by dermatological manifestations like maculopapular rash, typically disseminated on the trunk and the proximal portion of limbs, involvement of the oral mucosa and genital condyloma lata [1, 13]. The lesions are highly infectious [3, 13]. The latter is a papular skin lesion typical of secondary syphilis, observed in approximately 6-23% of patients diagnosed with this disease [13-15]. Lesions result from the coalescence of papules that may appear throughout the body, especially on moist areas such as skin folds, the perioral region or the perineal region [14], like in our patients.
The fact that condyloma lata may resemble condyloma acuminatum, poses a diagnostic challenge for clinicians, especially because the chancre lesions of primary syphilis may remain unnoticed for up to 50% of women [14, 16], particularly in the case of extragenital lesions, such as the rare case of nipple syphiloma caused by contact, biting, nibbling or trauma to the nipple during sexual intercourse [17], where exploration is particularly important. Secondary syphilis can be difficult to diagnose because the skin lesions may resemble other dermatologic conditions; it is important to be aware of this possibility and to perform a thorough examination to rule out other potential causes [3].
The delay in diagnosis, as in the first case presented, is due to the diverse presentations that can simulate other diseases, and the fact that clinicians may not request serological tests [18]. This delay is particularly important in cases of syphilis during pregnancy due to the potential maternal-fetal involvement [19].
The occurrence of secondary syphilis is rare and requires mandatory reporting and comprehensive patient follow-up. They have been described in 9-44% of syphilis cases [9].
Syphilis and HIV are two systemic, sexually transmitted diseases that share common risk factors [20], syphilis-HIV coinfection is very common, though for these reasons, we need to test for HIV. Due to the duration of the HIV window period, detecting possible coinfection in a patient requires ongoing follow-up. Both patients tested negative for HIV after the corresponding window period, thus coinfection was ruled out.
In both cases, the LGTPU and the IDU collaborated to design a suitable treatment, and we emphasized the importance of informing the patients’ sexual partners. Fortunately, in both women, the lesions have resolved. The first patient was considered healed, and the second patient is still being monitored at the IDU and showed a positive progression of the disease after treatment.
Strengths and limitations
The case reports presented here provide clinical insights into the manifestation, diagnosis, and management of secondary syphilis with vulvar condyloma lata. The descriptions include patient histories, physical examinations with accompanying images, diagnostic procedures, treatment regimens, and follow-up outcomes. Collaboration between gynecology, infectious diseases, and pathology ensures a comprehensive approach to patient care. Clear documentation of treatment responses provides valuable insights into therapeutic effectiveness. However, the limited sample size of only two cases restricts the generalizability of outcomes. The findings, while informative, may not be universally applicable, given the variability in patient demographics and clinical presentations. Addressing these limitations could enhance the robustness and relevance of the observations for a wider patient population. This highlights the significance of identifying, reporting, and treating vulvar condyloma lata to prevent further complications.
In conclusion, it is clinically important to identify, report, and treat condyloma lata to prevent further complications or progression to tertiary syphilis.
Learning points
Syphilis incidence is increasing worldwide. In the presence of vulvar lesions, the diagnosis of secondary syphilis can be challenging. Condyloma lata is a typical but very uncommon form of secondary syphilis.
Acknowledgments
The authors thank the patient for her informed consent to the publication of this clinical case. We thank the Fundacion Canaria Instituto de Investigacion Sanitaria de Canarias for its support.
Financial Disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors report no conflict of interest.
Informed Consent
Written informed consent was obtained from both patients for publication of this case report and accompanying images.
Author Contributions
NFMR and JLSM: clinical management of patients. EPEG, SNDRL and EBSM: writing and editing the manuscript. EPEG: writing, editing the manuscript. FGP: obtaining pathology images, analyzing and editing them. AIMM: supervising and reviewing the manuscript.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Tudor ME, Al Aboud AM, Leslie SW, Gossman W. Syphilis. In: StatPearls. Treasure Island (FL) ineligible companies. 2024.
pubmed - Arando Lasagabaster M, Otero Guerra L. Syphilis. Enferm Infecc Microbiol Clin (Engl Ed). 2019;37(6):398-404.
doi pubmed - Singh AE, Romanowski B. Syphilis: review with emphasis on clinical, epidemiologic, and some biologic features. Clin Microbiol Rev. 1999;12(2):187-209.
doi pubmed pmc - Detailed STD Facts - Syphilis [Internet]. 2023 [cited Mar 2, 2024]. Available from: https://www.cdc.gov/std/syphilis/stdfact-syphilis-detailed.htm.
- Monu A, Andrese E, Mihaela P, Toader P, Loghin L, Solovastru L, et al. Preventive medicine - laboratory epidemiological aspects of syphilis. 2020.
- Trovato E, Tognetti L, Campoli M, Cinotti E, Rubegni P. Syphilis diagnosis and treatment: state of the art. EMJ [Internet]. 2021 [cited Mar 27, 2024]; Available from: https://www.emjreviews.com/dermatology/article/syphilis-diagnosis-and-treatment-state-of-the-art/.
- Whiting C, Schwartzman G, Khachemoune A. Syphilis in dermatology: recognition and management. Am J Clin Dermatol. 2023;24(2):287-297.
doi pubmed pmc - Syphilis [Internet]. [cited Dec 26, 2023]. Available from: https://www.who.int/news-room/fact-sheets/detail/syphilis.
- Deshpande DJ, Nayak CS, Mishra SN, Dhurat RS. Verrucous condyloma lata mimicking condyloma acuminata: An unusual presentation. Indian J Sex Transm Dis AIDS. 2009;30(2):100-102.
doi pubmed pmc - Schmidt R, Carson PJ, Jansen RJ. Resurgence of syphilis in the United States: an assessment of contributing factors. Infect Dis (Auckl). 2019;12:1178633719883282.
doi pubmed pmc - Pinchera B, Viceconte G, Buonomo AR, Zappulo E, Mercinelli S, Moriello NS, et al. Epidemiological and clinical features of syphilis in the 21st century: A seven-year observational retrospective study of outpatients. Clinical Epidemiology and Global Health. 2022;16:101100.
- Resultados_Vigilancia_Sífilis [Internet]. [cited Dec 26, 2023]. Available from: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Paginas/Resultados_Vigilancia_S%C3%ADfilis.aspx.
- Walkty A, Shute L, Hamza S, Embil JM. Condyloma lata. IDCases. 2021;26:e01321.
doi pubmed pmc - Pourang A, Fung MA, Tartar D, Brassard A. Condyloma lata in secondary syphilis. JAAD Case Rep. 2021;10:18-21.
doi pubmed pmc - Mullooly C, Higgins SP. Secondary syphilis: the classical triad of skin rash, mucosal ulceration and lymphadenopathy. Int J STD AIDS. 2010;21(8):537-545.
doi pubmed - Gullette D, Hopkins K. Syphilis - an elusive diagnosis. The Journal for Nurse Practitioners. 2021;17(10):1189-1193.
- Michelerio A, Tomasini C. A crusted ulcer of the nipple. J Dtsch Dermatol Ges. 2023;21(11):1417-1420.
doi pubmed - Tsan GL, Claiborne RT. Ocular syphilis. Clin Exp Optom. 2021;104(7):756-759.
doi pubmed - Fang J, Partridge E, Bautista GM, Sankaran D. Congenital syphilis epidemiology, prevention, and management in the United States: a 2022 update. Cureus. 2022;14(12):e33009.
doi pubmed pmc - Wu MY, Gong HZ, Hu KR, Zheng HY, Wan X, Li J. Effect of syphilis infection on HIV acquisition: a systematic review and meta-analysis. Sex Transm Infect. 2021;97(7):525-533.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
