| Journal of Clinical Gynecology and Obstetrics, ISSN 1927-1271 print, 1927-128X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Gynecol Obstet and Elmer Press Inc |
| Journal website https://www.jcgo.org |
Original Article
Volume 12, Number 1, March 2023, pages 1-7
What Are the Top Benefits of a Prenatal Diagnosis of Fetal Esophageal or Intestinal Atresia?
Iglika Ivancheva Simeonova-Brachota, d, e, Marion Larroqueb, d, Fabrice Pierrea, Xavier Fritela, Valerie Vequeau-Gouaa, Guillaume Levardc
aDepartment of Obstetrics and Gynecology, Centre Hospitaler Universitaire de Poitiers, France
bDepartment of Obstetrics and Gynecology, Centre Hospitalier de La Rochelle, France
cDepartment of Paediatric Surgery, Centre Hospitalier Universitaire de Poitiers, France
dThese authors contributed equally to this article.
eCorresponding Author: Iglika Ivancheva Simeonova-Brachot, Service de Gynecologie- Obstetrique, Centre Hospitalier Universitaire de Poitiers, 86021 Poitiers Cedex, France
Manuscript submitted January 5, 2023, accepted February 13, 2023, published online March 31, 2023
Short title: Diagnosis of Fetal Esophageal or Intestinal Atresia
doi: https://doi.org/10.14740/jcgo833
| Abstract | ▴Top |
Background: The aim of the study was to investigate how prenatal diagnosis of fetal esophageal or intestinal atresia impacts obstetric and neonatal outcomes.
Methods: This was a retrospective cohort study of mothers and their neonates affected by fetal esophageal or intestinal atresia and followed in our center. The study population comprised 29 mothers and their fetuses (57%) identified prenatally, and 22 mothers and their neonates (43%) diagnosed postnatally.
Results: There was no significant difference between the two groups in induction of labor or mode of delivery. In the prenatal group, there was significantly higher prevalence of preterm birth before 37 and 34 weeks (59% vs. 31% and 24% vs. 0%, respectively) with no significant differences in rates of hospitalizations in a high-risk maternity unit and severe polyhydramnios (24% vs. 9% and 14% vs. 0%, respectively). Univariate regression analysis demonstrated that the only significant contribution to the prediction of delivery before 37 weeks was provided by prenatal diagnosis (R2 = 0.08, P = 0.046). Furthermore, we found no differences in age at surgery, neonatal complications and neonatal death. We observed significant differences in the duration of a neonatal intensive care unit stay (12 days (interquartile range: 41) vs. 6 (interquartile range: 4)).
Conclusions: We were not able to demonstrate any benefits of a prenatal diagnosis of fetal esophageal or intestinal atresia. This should reassure maternity care providers anytime such an unexpected delivery occurs.
Keywords: Atresia; Esophageal; Fetal; Intestinal; Prenatal
| Introduction | ▴Top |
Newborn infants with fetal esophageal, duodenal or intestinal atresia exhibit respiratory and nutritional problems in the early neonatal period [1-3]. In these cases, surgery is performed shortly after birth. Moreover, they need a clinical evaluation for any associated anomaly. Fetal esophageal, duodenal or intestinal atresia may be detected on a prenatal ultrasound scan. However, their diagnosis remains difficult and 50% are discovered postnatally because the related polyhydramnios is a third-trimester finding [4-6].
According to the CRACMO (The French Reference Center for Congenital Esophageal abnormalities), the prenatal diagnosis of fetal esophageal atresia requires delivery at a level 3 maternal care unit due to the need for immediate neonatal care [7].
The level 3 maternal unit provides obstetric and neonatal specialized care. It allows the performance of a pediatric surgery, including the management of esophageal, duodenal or intestinal atresia. Therefore, if the patient resides far from the referral unit, a decision of a scheduled delivery by induction the labor or by cesarean delivery should be made in advance [8]. Additionally, the upper gastrointestinal atresia is frequently complicated by polyhydramnios [9]. According to the Society for Maternal Fetal Medicine (SMFM) [10], in case of polyhydramnios, the choice of delivery mode is based on the standard obstetrics indications. However, compared to term pregnancies with normal amniotic fluid, pregnancies with polyhydramnios are found to be a risk factor for cesarean delivery and a non-reassuring fetal status [11, 12].
To the best of our knowledge, there have been only a few studies in the literature evaluating the impact of the antenatal diagnosis on the obstetric and neonatal outcomes specifically in cases of fetal esophageal or intestinal atresia, with or without hydramnios.
Most of the recent studies on the antenatal management of patients affected by fetal esophageal, duodenal or intestinal atresia focused predominantly on the neonatal outcomes [9]. Interestingly, less attention has been dedicated to the obstetric outcomes, although this is crucial for selecting the most appropriate management and detecting associated conditions that may have a substantial influence on neonatal outcomes. The aim of this study was to evaluate both obstetric and neonatal benefits and risks of a scheduled delivery at a level 3 of maternal care unit in the case of prenatally suspected esophageal, duodenal or intestinal atresia.
| Materials and Methods | ▴Top |
We conducted a retrospective cohort study at our prenatal diagnosis and pediatric surgery units between January 2009 and December 2019. We identified all pregnancies affected by fetal esophageal, duodenal or intestinal atresia referred to our prenatal diagnosis unit and all newborns managed for such atresia in our unit of pediatric surgery. We excluded cases with termination of pregnancy, stillbirth and false positive cases. Fifty-one out of a total of 77 consecutive mother-baby pairs met the exclusion criteria. The study population comprised 51 pregnancies, including 29 mothers (57%) and their 30 fetuses affected by prenatally diagnosed fetal atresia (there was one twin pregnancy with both twins affected), and 22 mothers (43%) and their 22 babies with postnatally diagnosed fetal atresia.
The study was approved by the CNIL (Commission Nationale de l’Informatique et des Libertes), approval number 2211250v0. The study was also registered with the ClinicalTrials.gov registry (NCT05362604). The study complied with the World Medical Association Declaration of Helsinki regarding ethical conduct of re-search involving human subjects.
Neonatal units in French hospitals are classified in three levels [13]. So that infants requiring high level care can receive it in a tertiary neonatal unit within the same network when appropriate, i.e., including a pediatric surgery team. The prenatal care of mothers with fetal esophageal or intestinal atresia includes obstetric consultation and level 3 ultrasound scheduled every 4 weeks at our unit until the end of the pregnancy, antenatal consultations with a specialized multidisciplinary team, and an antenatal visit to the birth center to reduce parental anxiety. We also provide a systematic antenatal psychological support for both parents as an integral component of the obstetrics follow-up.
We defined two groups of infants based on the prenatal diagnosis. The prenatal group comprised patients affected by confirmed fetal esophageal, duodenal or intestinal atresia and followed in our high-risk pregnancy unit, and scheduled for delivery between 38 and 39 weeks in our tertiary center, regardless of the patient’s place of residence. The postnatal group comprised patients with unsuspected fetal atresia who delivered in their local hospitals: their newborns were transferred to our tertiary hospital within 24 h and the mother had the option to be also transferred in order to accompany her baby.
Data were extracted from patient records, ultrasound reports, obstetric clinic visits, labor ward reports, and neonatal intensive care unit reports. We compared differences between prenatally and postnatally diagnosed atresia. Variables include gestational age at delivery, preterm delivery, induction of labor, mode of delivery, birth weight, age at surgery, length of hospital stay, neonatal complications, and neonatal death.
The definitions of polyhydramnios were maximal vertical pocket greater than or equal to 8 cm or amniotic fluid index greater than or equal to 24 cm. Severe polyhydramnios symptoms were managed by drainage of excess amniotic fluid. A cervix less than 25 mm was considered at high risk of preterm labor [14]. Small for gestational age at birth was defined as a newborn with a birth weight under the 10th percentile, adjusted for gestational age at delivery and by gender [15].
Distributions were tested for normality by the Kolmogorov-Smirnov test. Statistical comparisons were performed using the unpaired t-test for continuous variables, the Mann-Whitney U-test for not normally distributed data, and the Fisher exact and Chi-square tests for categorical variables. All analyses were two-tailed, and P < 0.05 was used to define statistical significance.
Logistic regression analysis was used to identify risk factors for preterm birth: the type of atresia, the presence of associated malformations or polyhydramnios and the total travel length. Kaplan-Meier survival curve was used to compare the gestational age at delivery, the duration of hospital stay and the duration of neonatal intensive care unit stay data in the two groups. The statistical software package SPSS 24.0 was used for data analysis.
| Results | ▴Top |
Analysis of the study population characteristics showed no significant difference in body mass index, parity, smoking status, and obstetric history (Table 1). We observed a higher maternal age in the prenatal group (difference in means = 2 years). The median gestational age of referral for level 3 ultrasound was 24 weeks (interquartile range (IQR): 22 - 32). In the prenatal group, the median travel length for obstetrics monitoring was significantly greater than that of the control group (661 km (IQR: 815) vs. 164 km (IQR: 180); P = 0.01).
 Click to view | Table 1. Maternal Clinical and Demographic Characteristics of the Study Population of Pregnant Women by Prenatal and Postnatal Diagnosis |
In the prenatal group (Table 2), delivery gestational age was lower by 2 weeks and there was a higher prevalence of preterm birth before 37 and 34 weeks (59% vs. 31%; P = 0.05 and 24% vs. 0%; P > 0.01, respectively). According to the Kaplan-Meier estimates (Fig. 1a), the median duration of pregnancy was lower in the prenatal group compared with the postnatal group. The resulting P value for log rank tests was 0.001. Univariate regression analysis (Table 3) demonstrated that only prenatal diagnosis provided a significant contribution to the prediction of delivery before 37 weeks (R2 = 0.08, P = 0.046). There was no significant difference in induction of labor and nor in the mode of delivery.
 Click to view | Table 2. Obstetric Outcomes of the Study Population of Fetuses by Prenatal and Postnatal Diagnosis |
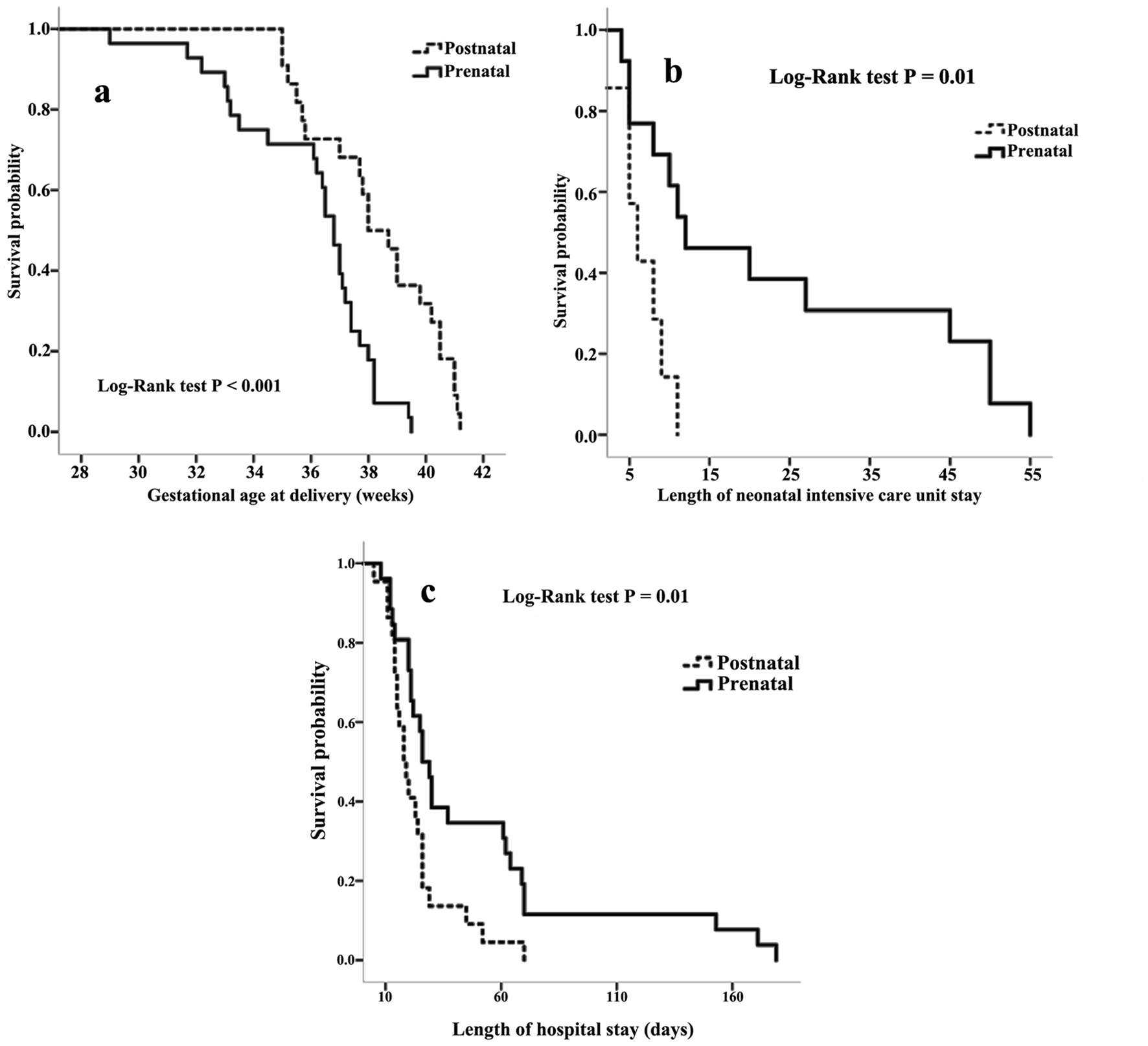 Click for large image | Figure 1. Kaplan-Meier survival curves demonstrating the gestational age of delivery (a), the duration of hospital stay (b) and the duration of neonatal intensive care unit stay (c) data in the postnatal group and prenatal group. |
 Click to view | Table 3. Univariable Regression Analysis in Prediction of Preterm Birth Before 37 Weeks |
The prenatal group had similar neonatal outcomes to the postnatal one. Table 4 shows no differences in age at surgery, neonatal complications and neonatal death. However, we found clinically significant differences in duration of hospital stay and neonatal intensive care unit stay in the prenatal group (28 days (IQR: 45) vs. 18 days (IQR: 12); P = 0.08 and 12 days (IQR: 41) vs. 6 days (IQR: 4); P = 0.02, respectively). According to the Kaplan-Meier estimates (Fig. 1b and c), the duration of hospital stay and the neonatal intensive care unit stay were higher in the prenatal group compared with the postnatal group. The resulting P values for the log rank tests were 0.01 and 0.01, respectively. We also found a higher prevalence of jejunoileal atresia in the prenatal group (46% vs. 14%; P = 0.02) and esophageal atresia in the postnatal group (31% vs. 68%; P = 0.06).
 Click to view | Table 4. Neonatal Outcomes of the Study Population of Fetuses by Prenatal and Postnatal Diagnosis |
| Discussion | ▴Top |
Here, we observed a significantly higher prevalence of preterm birth before 37 and 34 weeks in the prenatal group. It seems that this higher risk of preterm delivery was associated with the prenatal diagnosis.
The retrospective nature of the analysis and the use of routine clinical practice data explain some missing information. However, our center has uniform obstetrics, antenatal, pediatric and surgery practices. In addition, this is an original study on a rare pathology. Contrary to the few relevant studies in the literature which focused on the neonatal outcomes, we also analyzed the obstetrical outcomes.
These results agree with Garabedian et al and De Jong et al who found a lower delivery gestational age in the group of prenatal diagnosis of fetal esophageal atresia (5 and 12 days, respectively) [9, 16]. The population-based study from the French National Register for infants with esophageal atresia type A born from 2008 to 2014 confirmed that the gestational age at delivery was significantly higher in the postnatal group compared to the prenatal group (36 weeks (35 - 38) versus 34 weeks (32 - 36); P = 0.048) [17]. A prospective study of congenital duodenal obstruction comprising duodenal atresia or stenosis in the UK found an overall median gestational age at birth of 36 weeks (26 - 42) [18]. These findings could be explained by the more severe forms of esophageal atresia in the prenatal group. In fact, Garabedian et al [19] described a greater defect size (2 cm vs. 1.4 cm, P < 0.001) and De Jong et al [16] found a greater rate of polyhydramnios (53% vs. 27%; P = 0.04) in the prenatal group. As other authors have noticed, we observed no differences in the rate of associated anomalies between the antenatal and postnatal groups of esophageal atresia [20]. The antenatal diagnosis of esophageal atresia is still challenging even for experts and this could explain the disparity in the two groups. Though we found a higher prevalence of jejunoileal atresia in the prenatal group and esophageal atresia in the postnatal group, the regression analysis showed that the type of atresia did not provide a significant contribution to the prediction of preterm delivery. Furthermore, we did not find differences in the prevalence of high-risk maternity unit hospitalizations and severe polyhydramnios in the two groups.
We demonstrated that scheduled delivery was not associated with an increased risk for cesarean delivery and induction of labor. However, the overall cesarean section rate at the study was higher than the overall rate at our unit (40% vs. 17.9% all causes combined) [21]. This is in agreement with Zeino et al [11], who observed a higher cesarean delivery rate (45.4% versus 8%, P < 0.05), more inductions of labor and non-vertex presentations (forehead, bregma, face) (57.9% versus 27.8%; P < 0.05 and 7.8% versus 1%; P < 0.05, respectively) in a case of idiopathic polyhydramnios.
Further, we also found a higher duration of neonatal intensive care unit stay in the prenatal group. This result agrees with Schlee et al, who also report trends toward lower morbidity and shorter hospitalization periods in the out born group affected by esophageal atresia [22]. We infer that the longer hospital stay may be related to the higher prevalence of preterm birth in the prenatal group. We think that atresia severity may facilitate prenatal identification and diagnosis, and may also explain the higher duration of neonatal intensive care unit stay. Still, we found no statistically significant difference in age at surgery, duration of exclusive intravenous nutrition, surgical and neonatal complications, associated malformations, and neonatal death between the two groups. These findings are in disagreement with De Jong et al [16] who reported a higher mortality in the prenatal group. Garabedian et al [9] also found that the composite variable of morbidity (anastomotic esophageal leaks, recurrent fistula, stenosis) was higher in the prenatal diagnosis group (38.7% vs. 26.1%, P = 0.044). The last result may be explained by the higher prevalence of esophageal atresia and related thoracic surgery in this study.
Conclusion
We were not able to demonstrate any benefits of a prenatal diagnosis of fetal esophageal or intestinal atresia. In addition, we observe significantly more premature births and a higher length of neonatal hospital stay in the prenatal diagnosis group. Our experience shows no differences in neonatal outcomes regardless the time of the diagnosis. That should reassure maternity care providers anytime such an unexpected delivery occurs. However, as no pediatrician is permanently available to provide the first line of support at all level 1 and 2 obstetric units in France, we still recommend a scheduled delivery at a tertiary center in the case of antenatally suspected esophageal or intestinal atresia. Furthermore, we strongly encourage active participation of local maternal-fetal specialists and pediatrician in the obstetrics follow-up of these cases.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
All patients were given a copy of the full informed consent form.
Author Contributions
Conception and design: Iglika Ivancheva Simeonova-Brachot, Marion Larroque, Fabrice Pierre, and Guillaume Levard. Acquisition of data: Iglika Ivancheva Simeonova-Brachot and Marion Larroque. Analysis and interpretation of data: Iglika Ivancheva Simeonova-Brachot. Drafting of the manuscript: Iglika Ivancheva Simeonova-Brachot and Marion Larroque. Critical revision of the manuscript for important intellectual content: Iglika Ivancheva Simeonova-Brachot, Fabrice Pierre, Xavier Fritel, Valerie Vequeau-Goua, and Guillaume Levard. Statistical analysis: Iglika Ivancheva Simeonova-Brachot. Administrative technical or material support: Iglika Ivancheva Simeonova-Brachot and Marion Larroque. Supervision: Iglika Ivancheva Simeonova-Brachot.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Dingemann C, Eaton S, Aksnes G, Bagolan P, Cross KM, De Coppi P, Fruithof J, et al. ERNICA consensus conference on the management of patients with esophageal atresia and tracheoesophageal fistula: diagnostics, preoperative, operative, and postoperative management. Eur J Pediatr Surg. 2020;30(4):326-336.
doi pubmed - Grosfeld JL, Rescorla FJ. Duodenal atresia and stenosis: reassessment of treatment and outcome based on antenatal diagnosis, pathologic variance, and long-term follow-up. World J Surg. 1993;17(3):301-309.
doi pubmed - Touloukian RJ. Intestinal atresia and stenosis. Raffensperger JG, ed. Swenson's Pediatric Surgery. 2nd ed. Norwalk, CT: Appleton and Lange; 1993. p. 305-319.
- Pedersen RN, Calzolari E, Husby S, Garne E, EUROCAT Working group. Oesophageal atresia: prevalence, prenatal diagnosis and associated anomalies in 23 European regions. Arch Dis Child. 2012;97(3):227-232.
doi pubmed - Kilbride H, Castor C, Andrews W. Congenital duodenal obstruction: timing of diagnosis during the newborn period. J Perinatol. 2010;30(3):197-200.
doi pubmed - Shawis R, Antao B. Prenatal bowel dilatation and the subsequent postnatal management. Early Hum Dev. 2006;82(5):297-303.
doi pubmed - CRACMO. Protocole national de diagnostic et de soins (PNDS): atresie de l'aesophage. Perfect En Pediatrie. 2019;2(2):98-115.
doi - Sfeir R, Bonnard A, Khen-Dunlop N, Auber F, Gelas T, Michaud L, Podevin G, et al. Esophageal atresia: data from a national cohort. J Pediatr Surg. 2013;48(8):1664-1669.
doi pubmed - Garabedian C, Vaast P, Bigot J, Sfeir R, Michaud L, Gottrand F, Verpillat P, et al. [Esophageal atresia: prevalence, prenatal diagnosis and prognosis]. J Gynecol Obstet Biol Reprod (Paris). 2014;43(6):424-430.
doi pubmed - Society for Maternal-Fetal Medicine . Electronic address pso, Dashe JS, Pressman EK, Hibbard JU. SMFM Consult Series #46: Evaluation and management of polyhydramnios. Am J Obstet Gynecol. 2018;219(4):B2-B8.
doi pubmed - Zeino S, Carbillon L, Pharisien I, Tigaizin A, Benchimol M, Murtada R, Boujenah J. Delivery outcomes of term pregnancy complicated by idiopathic polyhydramnios. J Gynecol Obstet Hum Reprod. 2017;46(4):349-354.
doi pubmed - Luo QQ, Zou L, Gao H, Zheng YF, Zhao Y, Zhang WY. Idiopathic polyhydramnios at term and pregnancy outcomes: a multicenter observational study. J Matern Fetal Neonatal Med. 2017;30(14):1755-1759.
doi pubmed - Decrets n° 98-899 et n° 98-900 du 9 octobre 1998. Journal Officiel. 1998;235:15343-15348.
- Salomon LJ, Diaz-Garcia C, Bernard JP, Ville Y. Reference range for cervical length throughout pregnancy: non-parametric LMS-based model applied to a large sample. Ultrasound Obstet Gynecol. 2009;33(4):459-464.
doi pubmed - ADIPOG. Courbes de morphometrie standard. 2022. Available from URL: https://www.audipog.net/Courbes-morpho.
- de Jong EM, de Haan MA, Gischler SJ, Hop W, Cohen-Overbeek TE, Bax NM, de Klein A, et al. Pre- and postnatal diagnosis and outcome of fetuses and neonates with esophageal atresia and tracheoesophageal fistula. Prenat Diagn. 2010;30(3):274-279.
doi pubmed - Garabedian C, Bonnard A, Rousseau V, Sfeir R, Cracmo, Drumez E, Michaud L, et al. Management and outcome of neonates with a prenatal diagnosis of esophageal atresia type A: A population-based study. Prenat Diagn. 2018;38(7):517-522.
doi pubmed - Bethell GS, Long AM, Knight M, Hall NJ, Baps C. Congenital duodenal obstruction in the UK: a population-based study. Arch Dis Child Fetal Neonatal Ed. 2020;105(2):178-183.
doi pubmed pmc - Garabedian C, Sfeir R, Langlois C, Bonnard A, Khen-Dunlop N, Gelas T, Michaud L, et al. [Does prenatal diagnosis modify neonatal management and early outcome of children with esophageal atresia type III?]. J Gynecol Obstet Biol Reprod (Paris). 2015;44(9):848-854.
doi pubmed - Fallon SC, Ethun CG, Olutoye OO, Brandt ML, Lee TC, Welty SE, Ruano R, et al. Comparing characteristics and outcomes in infants with prenatal and postnatal diagnosis of esophageal atresia. J Surg Res. 2014;190(1):242-245.
doi pubmed - N'Doye Aicha. Quel peut etre l'apport de la classification de Robson dans l'analyse des pratiques d'une maternite a faible taux de cesarienne? Analyse retrospective de 17 ans. 2018; [Cited February 5, 2022] Available from URL: http://petille.univ-poitiers.fr/notice/view/62120.
- Schlee D, Theilen TM, Fiegel H, Hutter M, Rolle U. Outcome of esophageal atresia: inborn versus outborn patients. Dis Esophagus. 2022;35(8):doab092.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Gynecology and Obstetrics is published by Elmer Press Inc.
